MyHealth360
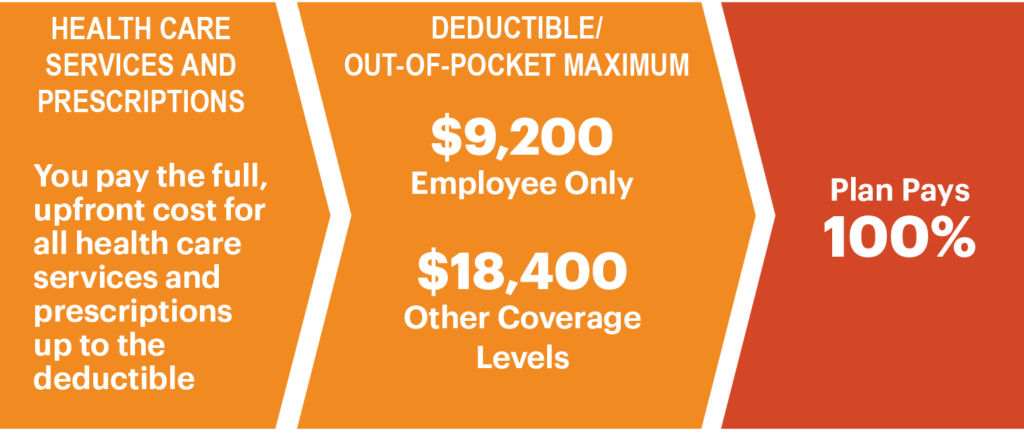
MyHealth360 provides a medical plan with access to prescription drug coverage. If eligible, you can select one of four coverage levels: Employee Only, Employee + Child(ren), Employee + Spouse/Domestic Partner or Family.
What to know
- Piedmont PRN Plan: If you are interested in enrolling or making changes to current elections, please complete the online enrollment form and return via email to PRNMedicalBenefits@piedmont.org
- The Piedmont PRN Plan provides medical and prescription drug coverage
- Prescription drugs are administered directly by Express Scripts
- Access to fertility, pregnancy and postpartum benefits and support for menopause and midlife care through Progyny (beginning Jan. 1, 2025)
- Medicare navigation support through SmartConnect at no cost to you
- Provider networks based on in- or out-of-network structure
- Participate in well-being activities to earn points to apply towards sweepstakes